Muscle pain that never fully goes away can be confusing and exhausting. If your body aches without a clear injury, you may have come across the term myalgia. Many people search for this word after months or years of unexplained muscle discomfort.
Inomyalgia is not yet an official medical diagnosis. However, it’s increasingly used to describe persistent deep muscle pain that doesn’t fit neatly into common conditions like simple myalgia or fibromyalgia. For many people, the term finally gives language to what they’re experiencing.
This guide explains myalgia in clear terms. You’ll learn what it means, why it happens, how it’s different from other pain disorders, and what actually helps.
What Is Inomyalgia?
Myalgia refers to chronic muscle pain that feels deep, widespread, and long-lasting. Unlike temporary soreness after exercise, this pain often persists for months. Sometimes it lasts for years.
The word itself combines:
-
“Myo” meaning muscle
-
“Algia” meaning pain
The added prefix is used to suggest internal or deep muscle involvement, not surface tenderness alone.
Key characteristics of myalgia
-
Pain is persistent, not occasional
-
Discomfort feels deep inside the muscles
-
No clear injury explains the symptoms
-
Standard tests often appear normal
People often feel frustrated because their pain is real, yet hard to prove through scans or lab results.
Is Inomyalgia a Recognized Medical Condition?
This is one of the most common questions.
Myalgia is not currently a formal diagnosis listed in major medical classification systems. Doctors don’t typically write it on official medical records.
However, that doesn’t mean the pain is imaginary.
Many clinicians use the term informally to describe chronic muscle pain patterns that don’t fully meet criteria for other disorders. It’s often discussed alongside conditions such as:
-
Fibromyalgia
-
Chronic myofascial pain
-
Central sensitization syndromes
Inomyalgia exists in a gray area between patient experience and formal medical labeling.
What Causes Inomyalgia?
There is no single cause. Most experts believe myalgia develops due to multiple overlapping factors.
1. Central nervous system sensitization
The brain and spinal cord may become overly sensitive to pain signals. Normal sensations start feeling painful.
This means:
-
Muscles aren’t necessarily damaged
-
The pain system is overreacting
2. Neurochemical imbalance
Low or irregular levels of neurotransmitters like serotonin and dopamine can reduce the body’s natural pain control.
This often explains why:
-
Pain worsens with stress
-
Mood and pain influence each other
3. Muscle energy dysfunction
Some researchers believe muscle cells may struggle to produce enough energy. This can cause:
-
Early fatigue
-
Burning or aching sensations
-
Slow recovery after activity
4. Chronic stress and trauma
Long-term stress keeps the body in a constant “fight or flight” mode. Muscles stay tense. Pain thresholds drop.
Past emotional or physical trauma can amplify this effect.
5. Poor sleep quality
Non-restorative sleep prevents muscle repair and nervous system reset. Pain becomes harder to control.
Common Symptoms of Inomyalgia
Symptoms vary from person to person. However, certain patterns appear frequently.
Physical symptoms
-
Deep muscle pain or aching
-
Muscle stiffness, especially in the morning
-
Tender areas without visible swelling
-
Muscle weakness without a clear cause
-
Sensation of heaviness in limbs
Systemic symptoms
-
Chronic fatigue
-
Poor exercise tolerance
-
Frequent headaches
-
Sleep disturbances
Cognitive and sensory symptoms
-
Brain fog or poor concentration
-
Sensitivity to pressure or touch
-
Discomfort with cold or heat
Pain may shift locations. One day it’s on the shoulders. Another day, it’s in the thighs or lower back.
How Is Inomyalgia Diagnosed?
There is no single test for myalgia. Diagnosis focuses on pattern recognition and exclusion.
Doctors usually follow these steps:
1. Detailed symptom history
Duration, location, triggers, and severity of pain matter more than one-time complaints.
2. Physical examination
Doctors check:
-
Muscle tenderness
-
Range of motion
-
Strength and posture
3. Rule-out testing
Blood tests and imaging help exclude:
-
Inflammatory diseases
-
Autoimmune disorders
-
Neurological conditions
When tests return normal, yet pain persists, clinicians may describe the condition amyalgiaia or a related chronic pain syndrome.
Inomyalgia vs Fibromyalgia: What’s the Difference?
These two are often confused.
| Feature | Inomyalgia | Fibromyalgia |
|---|---|---|
| Medical status | Descriptive term | Formal diagnosis |
| Pain focus | Deep muscle fibers | Widespread soft tissue |
| Tender points | Localized | Widespread |
| Cognitive symptoms | Sometimes | Very common |
| Diagnostic criteria | Informal | Established |
Myalgia may represent an early or muscle-dominant form of chronic pain. Fibromyalgia involves broader nervous system dysfunction.
Does Inomyalgia Get Worse Over Time?
Not always.
For some people, symptoms remain stable. For others, pain fluctuates depending on:
-
Stress levels
-
Sleep quality
-
Physical activity
-
Emotional health
Without proper management, flare-ups may become more frequent. With the right approach, many people experience significant improvement.
Effective Treatment Options for Inomyalgia
There is no one-size-fits-all cure. The most successful plans combine several strategies.
1. Gentle movement and physical therapy
Complete rest usually makes symptoms worse.
Helpful options include:
-
Walking
-
Stretching
-
Swimming
-
Light resistance training
The key is slow progression, not intensity.
2. Medications
Doctors may prescribe:
-
Pain modulators rather than strong painkillers
-
Low-dose antidepressants for nerve regulation
-
Muscle relaxants in selected cases
Medication works best when combined with lifestyle changes.
3. Sleep optimization
Improving sleep can reduce pain dramatically.
Helpful habits:
-
Fixed sleep schedule
-
Limiting screen time before bed
-
Creating a cool, dark sleep environment
4. Stress management
Stress directly amplifies pain signals.
Effective methods include:
-
Mindfulness practices
-
Breathing exercises
-
Cognitive behavioral therapy
-
Gentle yoga
5. Complementary therapies
Some people benefit from:
-
Massage therapy
-
Acupuncture
-
Heat therapy
-
Hydrotherapy
These don’t cure myalgia but can reduce symptom severity.
Daily Life Tips for Managing Inomyalgia
Small changes make a big difference.
-
Pace activities instead of pushing through pain
-
Break tasks into shorter sessions
-
Use heat for stiffness and cold for flare-ups
-
Maintain regular hydration
-
Track triggers in a simple pain journal
Consistency matters more than perfection.
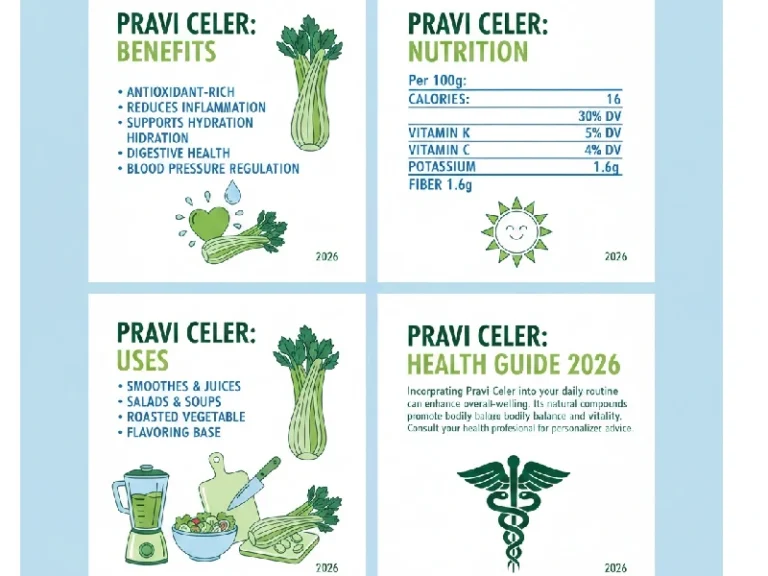
Can Diet Help Inomyalgia?
Diet won’t cure myalgia. However, it can influence inflammation and energy levels.
Many people report improvement with:
-
Balanced meals
-
Reduced processed foods
-
Adequate protein intake
-
Stable blood sugar levels
Listening to your body matters more than strict rules.
When Should You See a Doctor?
You should seek medical advice if:
-
Pain lasts longer than three monthsMuscle weakness worsens
-
Sleep becomes severely disrupted
-
Daily activities become difficult
Early support helps prevent long-term disability.
Frequently Asked Questions (FAQ)
What exactly is inomyalgia?
Myalgia describes chronic, deep muscle pain that persists without clear injury or inflammation and often involves nervous system sensitivity.
Is myalgia the same as muscle soreness?
No. Muscle soreness is temporary and activity-related. Myalgia is persistent and often unrelated to recent exertion.
Can myalgia be cured?
There is no single cure. However, many people achieve long-term symptom control with proper management.
Does exercise make myalgia worse?
Intense exercise can worsen symptoms. Gentle, gradual movement usually improves pain over time.
Is myalgia dangerous?
Myalgia is not life-threatening. However, it can significantly impact quality of life if untreated.
Final Thoughts
Myalgia describes a real and challenging experience. Even without a formal label, the pain deserves attention and care. Understanding the condition helps reduce fear and opens the door to effective management.
With the right combination of movement, rest, stress control, and medical guidance, many people regain function and comfort.